Federal Improper Payments Show Slight Decline in FY 2017
Published: February 01, 2018
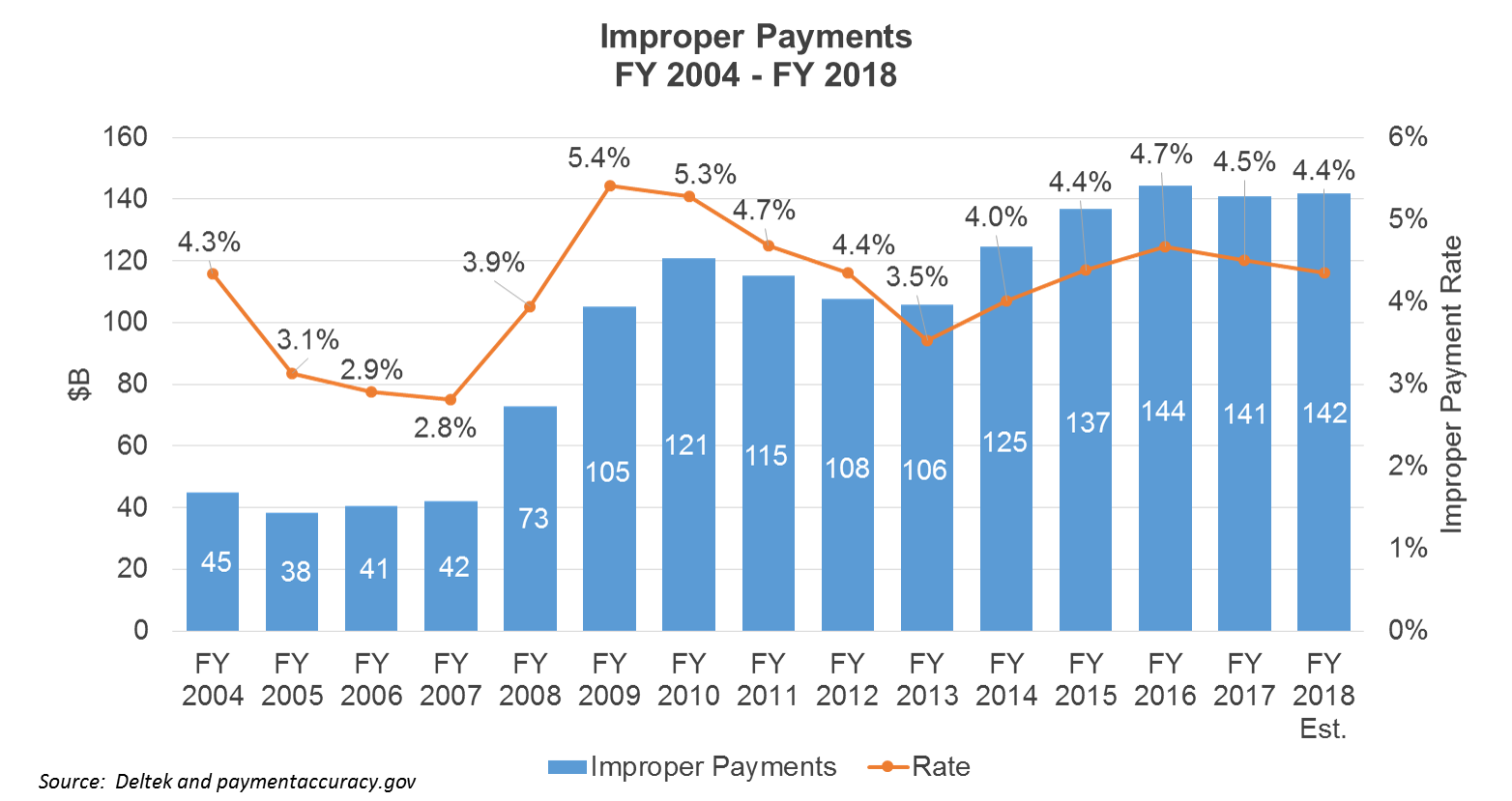
Total federal improper payments fell slightly to $141 billion in FY 2017 according to data recently released on paymentaccuracy.gov. The improper payment rate also dropped from 4.7% of program outlays in FY 2016 to 4.5% in FY 2017, amounting to a $3.6 billion decline over FY 2016 levels.
The federal government defines an improper payment as any payment that should not have been made or that was made in an incorrect amount under statutory, contractual, administrative, or other legally applicable requirements. Improper payments include overpayments or underpayments that are made to eligible recipients, payments made to ineligible recipients, payments made for ineligible goods or services, and payments for goods or services not received.
Total improper payments and payment rates declined from FY 2009 to FY 2013, but rose steadily from FY 2014 through FY 2016. The decline in FY 2017 is the first drop in both improper payment amounts and rates since FY 2013.
The decrease in FY 2017 improper payments was mostly attributable to the Medicare Fee-for-Service (FFS) program where improper payments dropped from $41.1 billion in FY 2016 to $36.2 billion in FY 2017, equating to an improper payment rate decrease of 11% to 9.5% of program outlays. This decrease occurred even while total program outlays increased due to an aging population reliant on Medicare benefits.
Distribution of improper payments by agency is charted below:
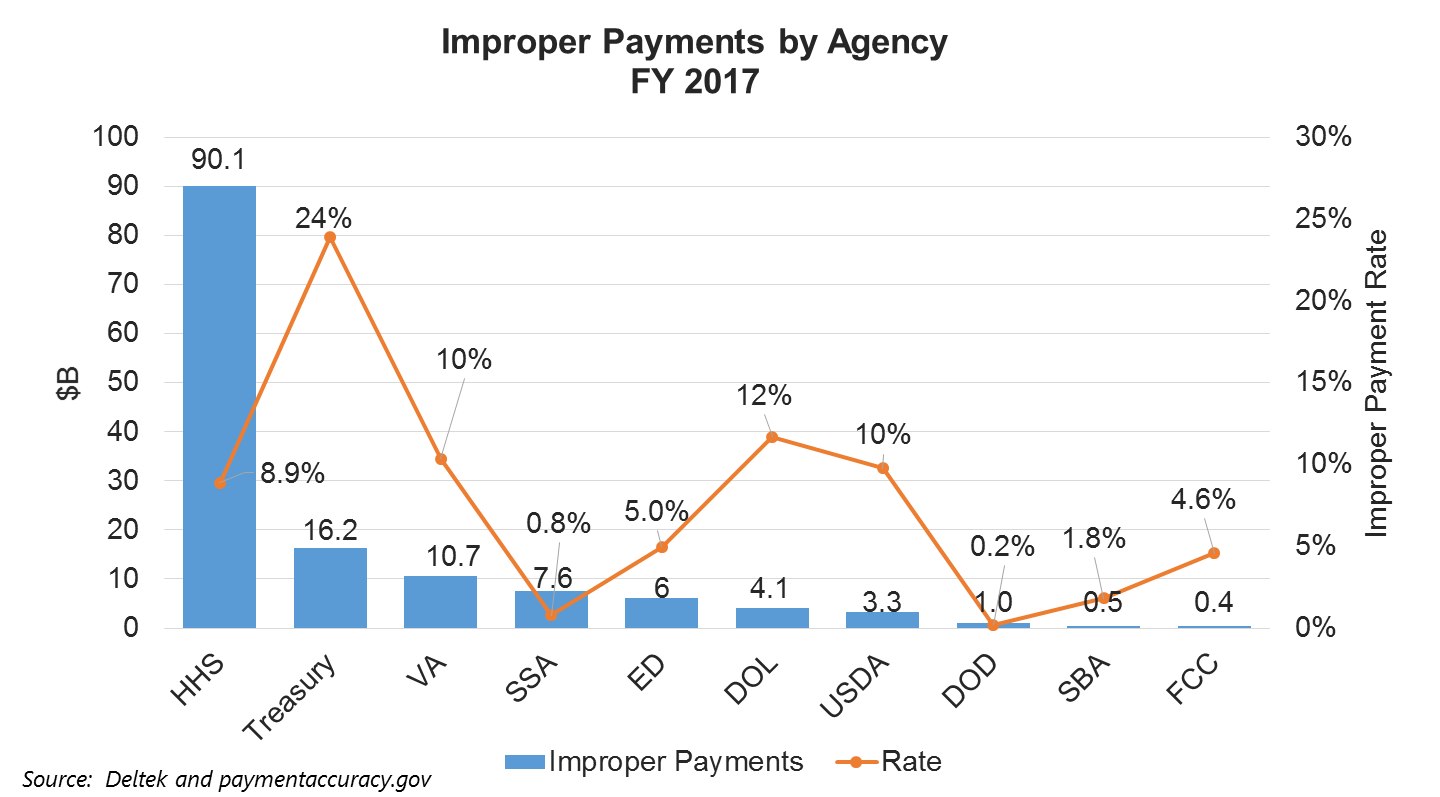
HHS continues to show the highest improper payment rates at 8.9% of total program outlays for FY 2017, equating to $90.1 billion.
In FY 2017, Medcaid outpaced the Medicare FFS program for the largest improper payment totals at $36.7B and a rate of 10.1% of total program outlays. The Medicare FFS program shows the second largest improper payment amount at $36.2B with a 9.5% improper payment rate. However, the program has shown progress increasing program integrity and reducing improper payments since FY 2014 with a $9.5 billion drop in improper payments and a 3.2% decrease in improper payment rates.
Main causes for improper payments for FY 2017 are shown below:

Most improper payments are due to administrative or process errors made by the federal agency, state or local agency, or other party. These types of errors are caused by incorrect data entry, classifying, or processing of applications or payments. The second most frequent cause of improper payments is insufficient documentation to determine if the payment is actually improper. This occurs when there is a lack of supporting documentation necessary to verify the accuracy of a payment identified in the improper payment testing sample. For example, a program does not have documentation to support a beneficiary's eligibility for a benefit.
Although improper payment amounts rose from FY 2014 to FY 2016, the decline in FY 2017 is encouraging. Also agencies continue to increase recovery amounts. The federal government recovered overpayments of $21.6 billion in FY 2017 up from $20.8 billion in FY 2016.
The Trump administration has made combating waste, fraud and abuse in federal programs a high priority. The administration and federal agencies continue to explore new and innovative ways to address the problem, leading to contractor opportunities in the areas of prescreening, big data, analytics, recapture audits, ID authentication, data warehousing, data authentication, predictive modeling, forensic accounting, and fraud case management.